treatment liver cancer
Treatment Options for Liver Cancer
Liver cancer, a serious disease, requires comprehensive understanding of available treatment liver cancer options. This guide explores various approaches, focusing on their effectiveness, side effects, and suitability for different stages of the disease. We'll examine surgical options, chemotherapy, radiation therapy, targeted therapy, immunotherapy, and palliative care, empowering you to make informed decisions in consultation with your healthcare provider. Remember, early diagnosis and prompt treatment liver cancer significantly improve outcomes.
Understanding Liver Cancer
Types and Stages of Liver Cancer
Liver cancer encompasses several types, the most common being hepatocellular carcinoma (HCC). Staging, crucial for determining treatment liver cancer strategies, classifies the cancer's extent and spread. Stages range from I (localized) to IV (metastatic), impacting the chosen treatment approach. Accurate staging requires a combination of imaging tests (ultrasound, CT scan, MRI) and potentially a biopsy.
Factors Influencing Treatment Decisions
Treatment selection for treatment liver cancer is personalized and depends on several critical factors: the type and stage of liver cancer, the patient's overall health and liver function, the presence of other medical conditions, and personal preferences. Consulting with a hepatologist and oncologist is vital to developing a tailored treatment plan.
Treatment Options for Liver Cancer
Surgical Options
Surgery, suitable for early-stage treatment liver cancer, aims to remove the cancerous tissue. This may include partial hepatectomy (removal of part of the liver) or liver transplantation (replacing the entire liver). The feasibility of surgery depends on the size, location, and extent of the tumor, as well as the patient's liver function. Post-surgery recovery varies depending on the extent of the procedure and individual health.
Chemotherapy
Chemotherapy, employing drugs to kill cancer cells, is often used for advanced-stage treatment liver cancer or to shrink tumors before surgery. Several chemotherapy regimens exist, each with specific side effects, such as nausea, fatigue, and hair loss. The effectiveness of chemotherapy in liver cancer varies depending on the type and stage of the cancer.
Radiation Therapy
Radiation therapy uses high-energy radiation to destroy cancer cells. It may be used alone or in combination with other treatment liver cancer methods like chemotherapy. External beam radiation is common, targeting the tumor from outside the body. Side effects can include skin irritation, fatigue, and digestive problems. The suitability of radiation therapy depends on the location and size of the tumor.
Targeted Therapy
Targeted therapy drugs focus on specific molecules involved in cancer cell growth. These medications can be more effective than traditional chemotherapy with fewer side effects. Examples include sorafenib and lenvatinib, often used for advanced treatment liver cancer. The effectiveness of targeted therapy depends on the specific genetic mutations present in the cancer cells.
Immunotherapy
Immunotherapy harnesses the body's immune system to fight cancer. It’s showing promise in treatment liver cancer, helping the body recognize and attack cancer cells. Different types of immunotherapy exist, including checkpoint inhibitors. Side effects vary but can include fatigue, skin rashes, and digestive issues.
Palliative Care
Palliative care focuses on improving the quality of life for patients with advanced liver cancer. It addresses pain, fatigue, and other symptoms, offering emotional and spiritual support. Palliative care can be provided alongside other treatment liver cancer methods and can significantly improve patient comfort and well-being.
Choosing the Right Treatment
Selecting the appropriate treatment liver cancer strategy necessitates a thorough evaluation of the individual's condition, encompassing the cancer's stage, overall health, and personal preferences. It's paramount to engage in open communication with the healthcare team, including oncologists, hepatologists, and palliative care specialists, to construct a personalized treatment plan that aligns with the patient's unique circumstances.
For comprehensive cancer care and cutting-edge research, consider exploring the resources available at the Shandong Baofa Cancer Research Institute.
Disclaimer: This information is for educational purposes only and should not be considered medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition.
Related products
Related products
Best selling products
Best selling products-
 Mark, a prostate cancer bone metastasis patient from the United States
Mark, a prostate cancer bone metastasis patient from the United States -
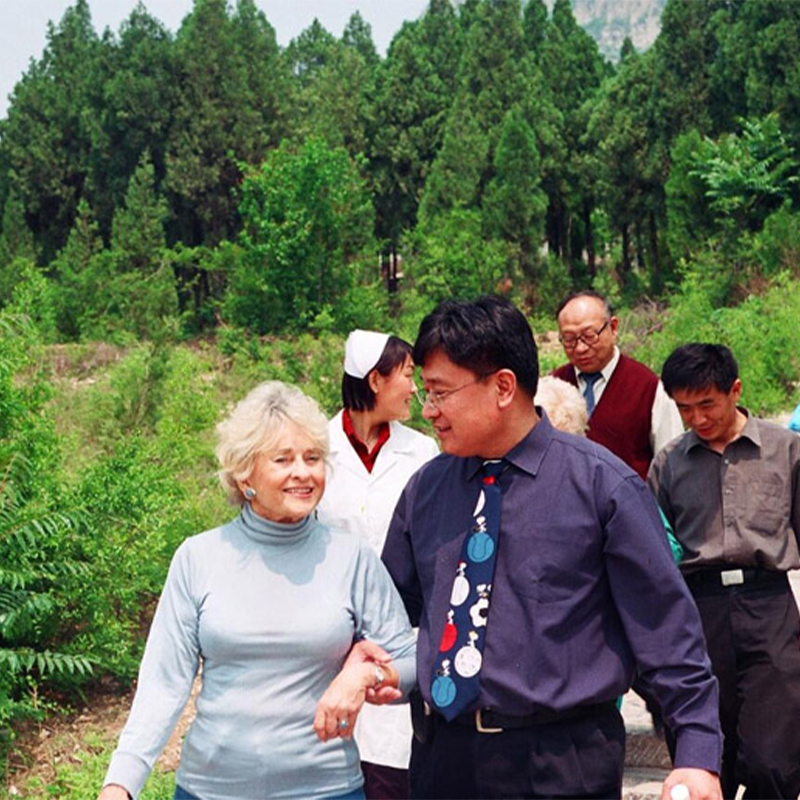 Famous American female painter Muriel
Famous American female painter Muriel -
 Andress, a 9-year-old boy from the United States
Andress, a 9-year-old boy from the United States -
 PAT, rectal cancer patient from the United States
PAT, rectal cancer patient from the United States -
 Anthony, lymphocytic cancer patient from the United States 24
Anthony, lymphocytic cancer patient from the United States 24 -
 Nell Smith, a throat cancer patient from Switzerland
Nell Smith, a throat cancer patient from Switzerland
Related search
Related search- treatment recurrent lung cancer treatment near me
- Cheap metastatic non small cell lung cancer treatment
- out of pocket cost for prostate cancer treatment Hospitals
- Cheap pancreatic cancer treatment near me
- treatment advances in lung cancer treatment Hospitals
- neuroendocrine lung cancer treatment cost
- China baofayu cost
- treatment gleason 7 prostate cancer treatment cost
- Cheap breast cancer test near me
- China Localized Drug Delivery for Cancer Hospitals